The National Academies of Science, Engineering, and Medicine has published a new report that acknowledges the challenges faced by hospitals that care for socio-economically challenged patients and offers suggestions for how to serve those patients more effectively.
The report, Systems Practices for the Care of Socially At-Risk Populations, is the second in a projected series of five reports on the subject.
The study notes that
Emerging evidence suggests that providers disproportionately serving patients with social risk factors for poor health outcomes may be more likely to fare poorly on quality rankings and to receive financial penalties, and less likely to receive financial rewards.
Because the study did not include any original empirical research and is based instead on literature reviews and case studies, the Academy declined to suggest best practices for serving this challenging population but did offer six recommendations for improving care to socio-economically disadvantaged communities:
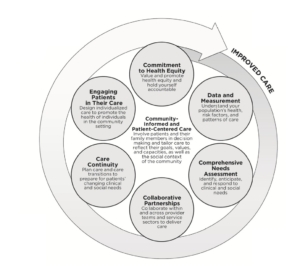
- Commitment to health equity. Value and promote health equity and hold yourself accountable.
- Data and measurement. Understand your population’s health, risk factors, and patterns of care.
- Comprehensive needs assessment. Identify, anticipate, and respond to clinical and social needs.
- Collaborative partnerships. Collaborate within and across provider teams and service sectors to deliver care.
- Care continuity. Plan care and transitions in care to prepare for patients’ changing clinical and social needs.
- Engaging patients in their care. Design individualized care to promote the health of individuals in the community setting.
The study also acknowledged the importance of adequate provider (primarily Medicare) payments in serving such a challenging population:
Both the availability of resources and alignment of financial incentives are prerequisites for the adoption and sustainability of these practices…Resources can provide the incentives to reduce disparities by targeting interventions at socially at-risk populations and incorporating equitable care and outcomes into accountability processes. Interventions that improve health and quality of care or reduce utilization and cost are only sustainable if the provider’s profits are higher with the intervention than without. Most of the efforts presented by the committee involve fixed costs and potentially shared benefits across multiple payers, so their economic feasibility depends on Medicare’s payment system and that of other payers. Environments in which a greater share of a provider’s revenue derives from payments related to health outcomes will make it more sustainable for them to invest in programs that improve quality and reduce cost.
 NAUH has long pointed to the special challenges of serving socio-economically disadvantaged communities and has frequently called on Medicare to improve how it pays hospitals that serve such communities.
NAUH has long pointed to the special challenges of serving socio-economically disadvantaged communities and has frequently called on Medicare to improve how it pays hospitals that serve such communities.
To learn more about what the Academy learned and what it has recommended, go here to see its news release accompanying publication of the report and go here to see the report itself.

