The following is the latest health policy news from the federal government for December 21 to January 4. Some of the language used below is taken directly from government documents.
No Surprises Act
HHS, the departments of Labor and the Treasury, and the Office of Personnel Management intend to reopen the comment period for submitting comments on a proposed rule governing federal Independent Dispute Resolution (IDR) operations. They plan to publish a notice to this effect in the near future with further details on reopening the comment period.
 Department of Health and Human Services
Department of Health and Human Services
- HHS’s Office of the National Coordinator for Health Information Technology (ONC) will issue the final “Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing” rule implementing the Electronic Health Record Reporting Program provision of the 21st Century Cures Act by establishing new Conditions and Maintenance of Certification requirements for health information technology developers under the ONC Health IT Certification Program. This final rule also will bring several updates of the certification criteria and standards recognized by the program. Program updates include revised certification criteria for “decision support interventions,” “patient demographics and observations,” and “electronic case reporting” as well as a new baseline version of the United States Core Data for Interoperability (USCDI) standard to Version 3. Additionally, this final rule provides enhancements to support information sharing under the information blocking regulations. The implementation of these provisions seeks to advance interoperability, improve algorithm transparency, and support the access, exchange, and use of electronic health information. This final rule also will update numerous technical standards in additional ways to advance interoperability, enhance health IT certification, and reduce burden and costs for health IT developers and users of health IT. Learn more from this preview version of the final rule, which is scheduled for official publication on January 9. The rule will take effect 30 days after official publication.
- HHS’s Health Resources and Services Administration (HRSA) has published the second of two planned notices informing the public of the availability of the complete lists of all geographic areas, population groups, and facilities designated as primary medical care, dental health, and mental health professional shortage areas (HPSA); the first such notice was published on July 3, 2023 and included HPSAs in a designated status and those proposed for withdrawal. Learn more about the lists and find links to them in this HRSA regulatory notice.
- HHS’s Health Resources and Services Administration (HRSA) sponsors four school-administered loan programs that give undergraduate and graduate schools funding to offer low, fixed-rate loans to students pursuing a wide range of health care careers. Learn more about the loan programs here. The deadline for applying to participate in the program is February 21.
- HRSA has published a new notice of funding to integrate behavioral health services into primary care settings using telehealth technology. HRSA will award approximately $8.75 million to up to 25 grantees over a period of five years. Public and private, non-profit, and for-profit entities that demonstrate they will provide services through a telehealth network are eligible to apply. Learn more from this HRSA notice, which also includes information about a January 17 technical assistance webinar, and from the grant notice. The deadline for applications is March 22.
- HHS and the General Services Administration have announced new guidance recommending that all federal facilities include overdose reversal medications, such as naloxone, in their safety stations on site. Learn more from this HHS news release and this regulatory announcement.
- HHS’s Agency for Health Care Research and Quality (AHRQ) has issued its annual report on health care quality and disparities to provide a comprehensive overview of the quality of care received by the general U.S. population and disparities in care experienced by different racial and socioeconomic groups. Go here for an introduction to the report and links to its individual sections, the entire report, and other resources.
- AHRQ seeks nominations of individuals to serve on the U.S. Preventive Services Task Force. Learn more about the task force, the professional background the agency seeks in potential nominees, and how to submit nominations from this AHRQ notice. The deadline for submitting nominations is March 15; those who are selected will begin their terms in January of 2025.
- HHS’s Office of the Inspector General has issued two favorable opinions regarding the use of a preferred hospital network as part of Medicare Supplemental Health Insurance (“Medigap”) policies. In such situations, an insurance company would contract with a preferred hospital organization to provide discounts on the otherwise-applicable Medicare inpatient deductibles for its policyholders and, in turn, would provide a premium credit of $100 off the next renewal premium to policyholders who use a network hospital for an inpatient stay. Find those opinions here and here.
Centers for Medicare & Medicaid Services
- CMS has issued a proposed rule implementing an order from a federal court that requires HHS to establish appeals processes for certain Medicare beneficiaries who are initially admitted as hospital inpatients but are subsequently reclassified as outpatients receiving observation services during their hospital stay and meet other eligibility criteria. The proposed rule includes processes for standard, expedited, and retrospective appeals. Learn more from this CMS announcement, which includes a link to the proposed rule. Comments are due by February 26.
- CMS and the CDC have issued a final rule updating the Clinical Laboratory Improvement Amendments of 1988 (CLIA) fees and clarifying CLIA fee regulations. The rule addresses a series of issues, including implementation of a process for sustainable funding for the CLIA program through a biennial two-part increase of CLIA fees; the incorporation of limited/specific laboratory fees; sanctions and more. Learn more about the final rule from this detailed CMS regulatory announcement. With specific, listed exceptions, the rule takes effect on January 27.
- CMS has published a bulletin on its January 2024 update of its ambulatory surgical center payment system. Affected providers include dentists, suppliers, and other providers billing for services delivered to Medicare patients. Find that bulletin here. The changes took effect on January 1.
- CMS has published two bulletins about billing requirements for intensive outpatient program services with new condition code 92. Affected providers include hospital outpatient departments, critical access hospitals, community mental health centers, and other providers that bill Medicare for intensive outpatient program services. Find those bulletins here and here. The changes took effect on January 1.
- From April to June 2023, CMS’s Center for Medicare and Medicaid Innovation hosted four meetings across the country to solicit feedback on promising practices and challenges to addressing health equity at the state and local levels. The agency intends to use what it learned from the sessions to inform its continuing implementation of its health equity initiative. Go here for a brief summary of the meetings and what they yielded.
- On November 16, CMS hosted a live Q&A session about the CMS Health Equity Confidential Feedback Reports for post-acute care providers that were released the previous month. Those reports stratified the Discharge to Community and Medicare Spending Per Beneficiary measures by dual-enrollment status and race/ethnicity. A recording of the webinar, slides, and a transcript can be found at the training web pages for home health, inpatient rehabilitation facilities, long-term-care hospitals, and skilled nursing facilities.
- CMS has issued notices alerting skilled nursing facilities, long-term-care hospitals, and inpatient rehabilitation facilities of upcoming measure removals from their respective quality reporting programs. Find those notices here.
- CMS has released an expanded Home Health Value-Based Purchasing technical expert panel report that presents a summary of the panel’s input on health equity approaches, performance measures, measure weights, and performance reporting. Find the report here.
- CMS is forming a technical expert panel to advise a contractor it has hired to collect stakeholder feedback for its ESRD Patient Life Goals Survey (PaLS) measure. The panel will hold one remote meeting of two to three hours sometime in February or March. Learn more about the panel and its expected work, the background CMS seeks in potential participants, and how to submit nominations from this CMS notice. The deadline for submitting nominations is January 12.
- CMS has published a bulletin clarifying the use of validation edits for providers with multiple service locations. Find that bulletin here.
 CMS has published a fact sheet that explains the performance year 2024 Merit-based Incentive Payment System (MIPS) policies for small practices (15 or fewer clinicians) that are changing or new and the performance year 2024 timeline. To find this fact sheet go here, scroll down to “Full Resource Library,” and click the link for “What’s New In 2024 For Small Practices” for the downloadable file.
CMS has published a fact sheet that explains the performance year 2024 Merit-based Incentive Payment System (MIPS) policies for small practices (15 or fewer clinicians) that are changing or new and the performance year 2024 timeline. To find this fact sheet go here, scroll down to “Full Resource Library,” and click the link for “What’s New In 2024 For Small Practices” for the downloadable file.- CMS has posted a guide to help small practices get started participating in MIPS during the 2024 performance period. To find this guide go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Quick Start Guide for Small Practices” for the downloadable file.
- CMS has published a user guide that provides details and screenshots for submitting data for traditional MIPS for the 2023 performance year. To find this guide go here, scroll down to “Full Resource Library,” and click the link for “2023 Traditional MIPS Data Submission User Guide” for the downloadable file.
- CMS has published forms detailing the measure methodology for the 27 episode-based cost measures, the MSPB Clinician measure, and the TPCC measure used for the MIPS Cost performance category in 2024. To find the forms go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Cost Measure Information Forms” for the downloadable zip file.
- CMS has posted a document that provides a summary of cost measures in use for the MIPS cost performance category in 2024 and measures under development. To find the document go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Summary of Cost Measures” for the downloadable file.
- CMS has published files that detail the codes used in the specifications for each of the 27 episode-based cost measures, the MSPB Clinician measure, and the TPCC measure that are in use for the MIPS Cost performance category in 2024. To find the files go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Cost Measure Codes List” for the downloadable zip file.
- CMS has published a document that describes methods for calculating the CMS Web Interface benchmarks for ACOs reporting the CMS Web Interface measures for the 2024 performance year. The benchmarks for the 10 CMS Web Interface measures are displayed in the appendix of this document. To find the document go here, scroll down to “Full Resource Library,” and click the link for “Performance Year 2024 APM Performance Pathway: CMS Web Interface Measure Benchmarks for ACOs” for the downloadable file.
- CMS has published a detailed overview of the requirements for the 2024 Promoting Interoperability performance category objectives and measures. To find the overview go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Promoting Interoperability Measure Specifications” for the downloadable zip file.
- CMS has published a guide to help clinicians participate in the Improvement Activities performance category of MIPS during the 2024 performance period. To find the guide go here, scroll down to “Full Resource Library,” and click the link for “2024 Improvement Activities Quick Start Guide” for the downloadable file.
- CMS has published a user guide that provides details and screenshots for submitting data for a MIPS Value Pathway (MVP) for the 2023 performance year. To find the guide go here, scroll down to “Full Resource Library,” and click the link for “2023 MVP Data Submission User Guide” for the downloadable file.
- CMS has published a user guide that provides details and screenshots for submitting data for the APM Performance Pathway (APP) for the 2023 performance year. To find the guide go here, scroll down to “Full Resource Library,” and click the link for “2023 APP Data Submission User Guide” for the downloadable file.
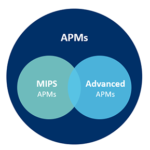
- CMS has posted a comprehensive list of APMs for the 2023 and 2024 performance period. To find the list go here, scroll down to “Full Resource Library,” and click the link for “2023 and 2024 Comprehensive List of APMs” for the downloadable file.
- CMS has published files that provide comprehensive descriptions of the 2023 CMS Web Interface measures for ACOs reporting the CMS Web Interface measures via the APM Performance Pathway (APP) for the 2023 performance year. To find the files go here, scroll down to “Full Resource Library,” and click the link for “Performance Year 2023 APM Performance Pathway: CMS Web Interface Measure Specifications and Supporting Documents for ACOs” for the downloadable zip file.
- CMS has published files that provide comprehensive descriptions of the 2024 CMS Web Interface measures for ACOs reporting the CMS Web Interface measures via the APM Performance Pathway (APP) for the 2024 performance year. To find the files go here, scroll down to “Full Resource Library,” and click the link for “Performance Year 2024 APM Performance Pathway: CMS Web Interface Measure Specifications and Supporting Documents for ACOs” for the downloadable zip file.
- CMS has published an FAQ about data submission via the CMS Web Interface. To find the FAQ go here, scroll down to “Full Resource Library,” and click the link for “2023 CMS Web Interface FAQs” for the downloadable file.
- CMS has published an explanation of the sampling methodology for the 10 clinical quality measures reported via the CMS Web Interface. To find the explanation go here, scroll down to “Full Resource Library,” and click the link for “2023 CMS Web Interface Sampling Methodology” for the downloadable file.
- CMS has published guidance for clinicians who are reporting CMS Web Interface measures for Medicare Shared Savings Program ACOs on how telehealth may relate to reporting measure data within the CMS Web Interface. To find the guidance go here, scroll down to “Full Resource Library,” and click the link for “2023 CMS Web Interface Telehealth Guidance” for the downloadable guidance.
- CMS has published a description of the process for assigning Medicare patients to a group, virtual group, subgroup, or APM Entity participating in MIPS in 2023. To find the explanation go here, scroll down to “Full Resource Library,” and click the link for “2023 CAHPS for MIPS Survey Assignment Methodology” for the downloadable file.
- CMS has posted documents that provide details on the measure specifications for the Multiple Chronic Care Conditions (MCC) Risk-Standardized Hospital Admission Rates for Patients for MIPS groups. To find the documents go here, scroll down to “Full Resource Library,” and click the link for “2024 All-Cause Unplanning Admissions for Multiple Chronic Conditions Measure” for the downloadable zip file.
- CMS has published information about the measure specifications for the Risk-Standardized Acute Cardiovascular-Related Hospital Admission Rates for Patients with Heart Failure under the MIPS groups with updates for the 2024 performance period. To find the information go here, scroll down to “Full Resource Library,” and click the link for “2024 Acute Cardiovascular-Related Admission Rates for Patients with Heart Failure Measure” for the downloadable zip file.
- CMS has published details about the measure specifications for the Risk-Standardized Complication Rate (RSCR) Following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) for MIPs with updates for the 2024 performance period. To find the information go here, scroll down to “Full Resource Library,” and click the link for “2024 Hip Arthroplasty and Knee Arthroplasty (THA/TKA) Complications Measure” for the downloadable zip file.
- CMS has published information about the measure specifications for the Hospital-Wide, 30- Day, All-Cause Unplanned Readmission (HWR) Rate for MIPS groups with updates for the 2024 performance period. To find the information go here, scroll down to “Full Resource Library,” and click the link for “2024 All-Cause, Unplanned Hospital-Wide Readmissions Measure” for the downloadable zip file.
- CMS has published a detailed list of the 2024 MIPS quality measures. The technical measure specifications and supporting documents for the 2024 MIPS quality measures are posted before the start of the performance year. To find the list go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Quality Measures List” for the downloadable file.
- CMS has published comprehensive descriptions of the 2024 claims measures for the MIPS quality performance category. To find the information go here, scroll down to “Full Resource Library,” and click the link for “2024 Medicare Part B Claims Measure Specifications and Supporting Documents” for the downloadable zip file.
- CMS has published comprehensive descriptions of the 2024 MIPS Clinical Quality Measures (CQMs) for the MIPS quality performance category. To find the information go here, scroll down to “Full Resource Library,” and click the link for “2024 MIPS Clinical Quality Measure Specifications and Supporting Documents” for the downloadable zip file.
- CMS has published instructions for using the associated Quality Payment Program JSON templates to submit the data collected for MIPS Clinical Quality Measures (CQMs) during the 2023 performance year. To find the instructions go here, scroll down to “Full Resource Library,” and click the link for “2023 QPP JSON Templates and Instructions” for the downloadable zip file.
- Clinicians, groups, and APMs that exceed one or two but not all three elements of the low-volume threshold can opt in to participate in MIPS. CMS has posted a guide describing how to elect to opt in or voluntary report for the 2023 performance year. To find the guide go here, scroll down to “Full Resource Library,” and click the link for “2023 MIPS Opt-In and Voluntary Reporting Election Guide” for the downloadable file.
HHS Newsletters
- CMS – MLN Connects – January 4
- AHRQ News Now – December 19
- HRSA eNews – January 4
- CMMI Evaluation Digest – December 2023
Food and Drug Administration
The FDA has updated its information for consumers on their treatment options if they contract COVID-19. Find that updated advice here.
 Stakeholder Events
Stakeholder Events
CMS – Guiding an Improved Dementia Experience (GUIDE) Model Webinar – January 11
CMS will hold a webinar to answer questions about the application process for its new Guiding an Improved Dementia Experience (GUIDE) Model on Thursday, January 11 at 2:00 (eastern). Go here to register to participate.
MedPAC – January 11-12
The Medicare Payment Advisory Commission (MedPAC) will hold its next public meeting on Thursday, January 11 and Friday, January 12. The meeting’s agenda and information about how to participate virtually have not yet been released but when they are they will be posted here.
CMS – Hospital Price Transparency Webinar – January 17
To help hospitals prepare for meeting new requirements for price transparency, CMS will hold a webinar on Wednesday, January 17 at 2:00 (eastern) to review the new requirements; to present examples of how to encode machine-readable file standard charge information in the template layout CMS will require hospitals to use; and to demonstrate its “GitHub” repository. Go here to register to participate.
MACPAC – January 25-26
The Medicaid and CHIP Payment and Access Commission will hold its next public meeting on Thursday, January 25 and Friday, January 26. The meeting’s agenda and information about how to participate virtually have not yet been released but when they are they will be posted here.
CMS – Health Equity Conference – May 29-30
CMS will hold its second annual CMS Health Equity Conference on Wednesday, May 29 and Thursday, May 30. The free, hybrid conference will be held in person in Bethesda, Maryland and available online for virtual participation and involve health equity leaders from federal and local agencies, health provider organizations, academia, community-based organizations, and others. Conference participants will hear from CMS leadership on recent developments and updates to CMS programs; explore the latest health equity research; discuss promising practices and creative solutions; and collaborate on community engagement strategies. Learn more from the conference web page.
Stakeholder Events: Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing (HTI-1) Final Rule
HHS’s Office of the National Coordinator for Health Information Technology (ONC) will host the following information sessions to explain the Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing (HT1-1) final rule.
HTI-1 Final Rule Insights Condition Information Session
Tuesday, January 9, 2024 at 3:00 pm (eastern) – register here
HTI-1 Final Rule Decision Support Interventions Information Session
Wednesday, January 17, 2024 at 1:00 pm (eastern) register here
HTI-1 Final Rule Information Blocking Information Session
Thursday, January 25, 2024 at 1:00 pm (eastern) – register here
HTI-1 Final Rule Overview with Question & Answer Information Session #2
Thursday, February 1, 2024 at 1:00 pm (eastern) – register here


 Stakeholder Events
Stakeholder Events